
PhysioEye Breakthrough: 4 Ways to End the Blind Spot of Longitudinal Mobility Assessment in Nursing Homes
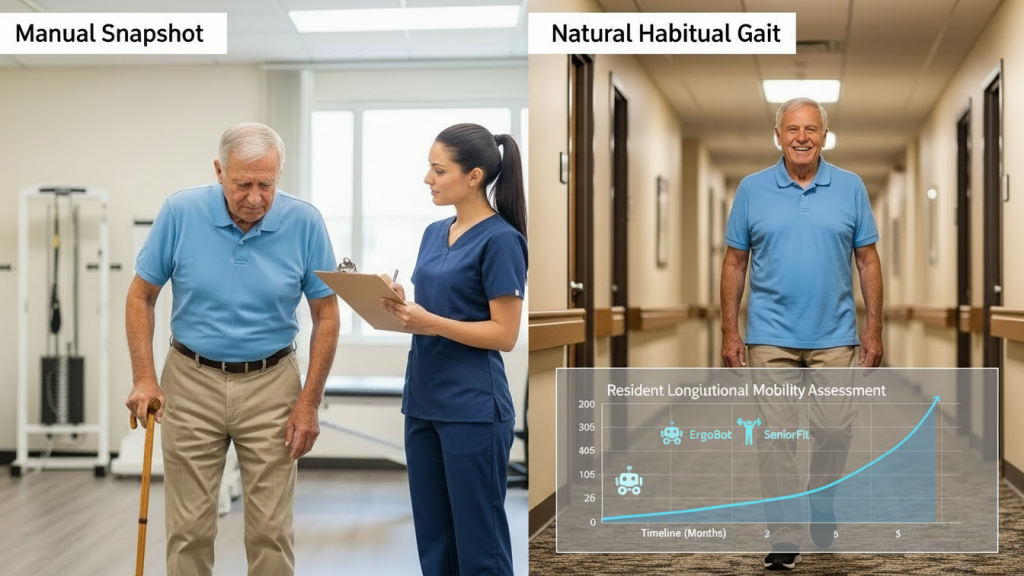
Longitudinal Mobility Assessment is the missing link in modern geriatric care, representing a shift from reactive “snapshot” checks to a continuous stream of actionable health intelligence. In the current care landscape, most facilities rely on manual, sporadic evaluations that fail to capture the subtle, day-to-day decline in resident health. By the time a visible change is noted by a caregiver, the risk of a catastrophic event has often already peaked. PhysioEye fixes this “blind spot” by introducing a fully Automated Mobility Assessment that provides the data necessary for a truly professional Longitudinal Mobility Assessment.
For Nursing Home Automation to be effective, it must do more than just record a single walk; it must map a resident’s physical journey over months and years. This is the core of Fall Prevention for Seniors: knowing that a resident’s step width has narrowed by 5% over the last thirty days, a detail only visible through a dedicated Longitudinal Mobility Assessment.
The Clinical Necessity of Longitudinal Mobility Assessment
In traditional settings, a physical therapist might perform an Elder Mobility Assessment once every quarter. However, clinical research suggests that mobility is not a static trait but a fluctuating “vital sign.” A single manual check cannot account for “good days” and “bad days,” leading to inaccurate care plans.
By utilizing PhysioEye, facilities can perform a Longitudinal Mobility Assessment every time a resident walks past a sensor. This high-frequency data collection allows for:
-
Early Detection of Frailty: Identifying a slow decrease in gait speed—a primary indicator of mortality.
-
Tracking Intervention Efficacy: Seeing exactly how Robotic Assisted Rehabilitation is improving a resident’s range of motion.
-
Refining Therapy: Adjusting Robotic Assisted Ergotherapy parameters based on the real-world performance captured in the Longitudinal Mobility Assessment.
Eliminating “Snapshot Bias” in Elder Care
Manual assessments suffer from what clinicians call “Snapshot Bias.” A resident might perform well during a scheduled test due to the “Hawthorne Effect” (improving behavior when being watched), only to struggle significantly in their daily routine. A Longitudinal Mobility Assessment removes this human error.
PhysioEye operates in the background of a Robotic Assisted Nursing Home, capturing natural movement. When this data is aggregated, the resulting Longitudinal Mobility Assessment provides a “trend line” that is far more reliable for medical decision-making than any single goniometer reading.
Securing Pflegegrad Accuracy with Trend Data
The financial health of a facility is tied directly to the Pflegegrad classification of its residents. Insurance auditors often look for proof of “permanent decline” to justify higher funding levels. A single Senior joint mobility assessment may be dismissed as an outlier, but a six-month Longitudinal Mobility Assessment report is undeniable.
With PhysioEye, you can generate automated reports that show the exact trajectory of a resident’s independence. By documenting the progressive need for Robotic Assisted Occupational Therapy, the Longitudinal Mobility Assessment becomes your facility’s strongest tool for revenue protection and audit defense.
Enhancing Fall Prevention through Predictive Trends
Falls rarely happen without warning; they are usually preceded by weeks of subtle kinematic changes. Our Automated Geriatric Fall Risk Assessment uses the power of Longitudinal Mobility Assessment to flag these changes before the fall occurs.
For example, a slight increase in “Double Support Time” (the time both feet are on the ground) is a classic sign of balance insecurity. While a human might miss a 0.1-second change, a Longitudinal Mobility Assessment powered by PhysioEye identifies it instantly. This allows the staff to intervene with SeniorFit programs or adjust the use of TrollyBot to provide extra support during peak fatigue hours.
Empowering the Modern Workforce
Staff shortages are the greatest challenge in European care today. Caregivers simply do not have the time to perform manual, repetitive tracking. By automating the Longitudinal Mobility Assessment, PhysioEye frees up hundreds of hours of staff time.
Instead of writing manual reports, your team can focus on the actual delivery of Robotic Assisted Rehabilitation. The Longitudinal Mobility Assessment acts as a “digital assistant” that watches the residents’ safety 24/7, ensuring that no resident “falls through the cracks” of a busy shift. This is the practical application of Nursing Home Automation—using technology to bring the “human” back into care.
Conclusion: The Future is Longitudinal
-
The physical toll on staff caring for Parkinson’s residents is immense. Manually stretching a rigid limb or supporting a resident during exercise leads to high rates of workplace injury. By shifting the physical labor to Robotic Assisted Rehabilitation, the human therapist is elevated to the role of a “Clinical Decision Maker.” They monitor the data and adjust the parameters, while the ErgoBot performs the heavy lifting. This is the ultimate promise of Nursing Home Automation: a safer environment for both the resident and the staff involved in Parkinson’s Rehabilitation.
The era of guessing is over. The “Blind Spot” in nursing homes has existed because we lacked the tools to see movement over time. Today, a Longitudinal Mobility Assessment is the gold standard for clinical safety and financial stability.
By integrating PhysioEye and tools like ErgoBot into your facility, you are choosing a data-driven future. Whether it is securing a higher Pflegegrad or perfecting your Fall Prevention for Seniors, the answer lies in the data. Start your journey toward a Robotic Assisted Nursing Home today and end the blind spot for good with a professional Longitudinal Mobility Assessment.
